Have you recently been diagnosed with PCOS or polycystic ovary syndrome? If your story is anything like mine, you were diagnosed and left to figure out everything on your own. Getting any diagnosis can be unsettling, and unfortunately, PCOS cannot be cured, but it can be managed with some assistance.

If you have never heard of polycystic ovary syndrome until now, let me give you a quick review! You would think that the name would give it all away, but did you know that people diagnosed with PCOS do not necessarily have to have polycystic ovaries to meet the diagnostic criteria? Also, the “cysts” are not cysts but antral follicles. That is why several name change proposals have highlighted that it is not just a reproductive problem but an endocrine-metabolic disorder with a unique set of symptoms.
How is polycystic ovary syndrome diagnosed?
There are several statements of diagnostic parameters that have been made for PCOS, and they are outlined below. As you read through the criteria, you can see why a name change is warranted. One name change proposal is “Hyperandrogenic Persistent Ovulatory Dysfunction Syndrome or HA-PODS” (Khadilkar, 2016).
NIH Statement (1990)
To include all the following:
1. Hyperandrogenism and/or hyperandrogenemia
– The state defines hyperandrogenism as excessive production and/or secretion of male sex hormones, which is usually manifested by acne, hirsutism, or male pattern baldness
– Hyperandrogenemia is defined by increased blood levels of male sex hormones with/without manifestations
2. Oligo-ovulation
– Oligo-ovulation is defined as irregular or infrequent ovulationExclusion of related disorders
ESHRE/ASRM Statement (The Rotterdam ESHRE/ASRM-sponsored PCOS consensus workshop group, 2004)
To include two of the following, in addition to the exclusion of related disorders:
1. Oligo-ovulation or anovulation (no ovulation)
2. Clinical and/or biochemical signs of hyperandrogenism (e.g., hirsutism, elevated serum total or free testosterone)
3. Polycystic ovaries (by ultrasonography) polycystic ovary as having 12 or more follicles, measuring between 2 and 9 mm, and/or an ovarian volume >10 cc
AES Suggested Criteria for the Diagnosis of PCOS (Azziz, 2006)
To include all of the following:
1. Hyperandrogenism: hirsutism and/or hyperandrogenemia
2. Ovarian dysfunction: oligo-ovulation and/or polycystic ovaries
3. Exclusion of other androgen excess or related disorders
**TIP: “Other reasons for androgen excess include congenital adrenal hyperplasia (which accounts for up to 9 percent of cases of androgen excess), high prolactin, and hormonal birth control with a high androgen index (testosterone-like progestin)” (Briden, 2022)
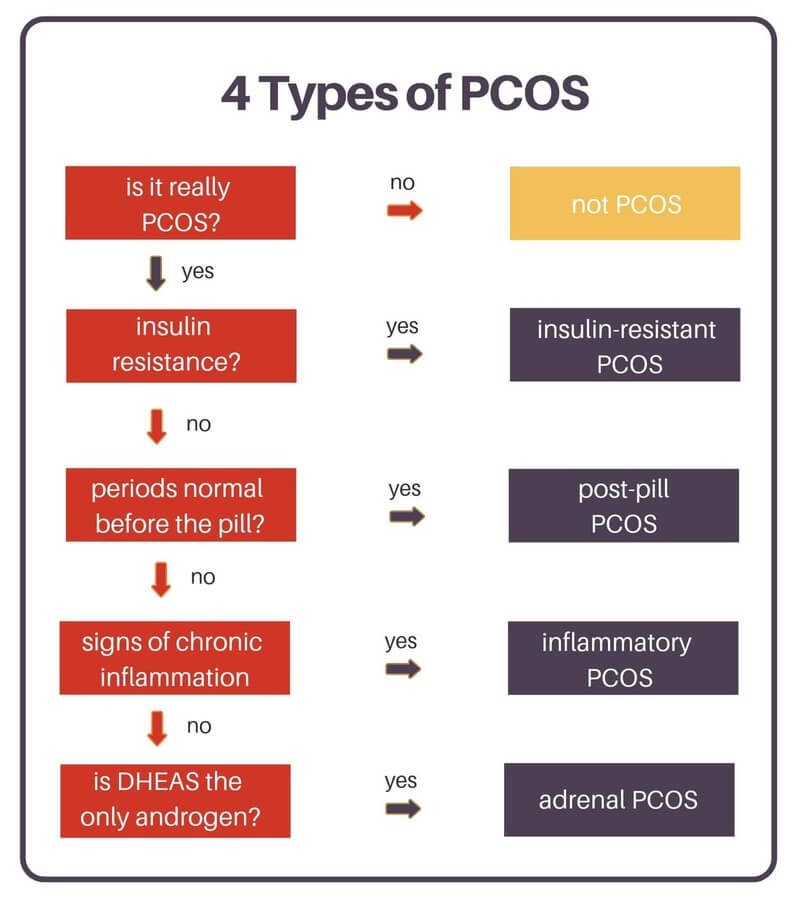
What are the Four types of PCOS?
Once you get the diagnosis of PCOS, it is an umbrella term and does not address or make conclusions on the root cause of your diagnosis. Despite continued research, PCOS is still ill-understood, but some gains have been made toward understanding the drivers of PCOS. The four drivers of PCOS are Insulin-resistant, post-pill, inflammatory, and adrenal.
| Insulin resistant PCOS | – Most common – Cells are resistant to insulin – Higher levels of circulating insulin lead to higher levels of androgens and anovulation – Risk factors: smoking, excess sugar intake, excess trans-fat intake, environmental toxins |
| Post-Pill PCOS | – Hormonal birth control stops ovulation – Prolonged anovulation after stopping hormonal birth control – Risk Factors: taking hormonal birth control |
| Inflammatory PCOS | – Inflammation impedes ovulation, disrupts hormone receptors, and stimulates adrenal androgens such as DHEA and androstenedione (Briden, 2014) – Risk factors: unaddressed autoimmune disorders, stress, environmental toxins, intestinal permeability, and inflammatory foods |
| Adrenal PCOS (Briden, 2014) | – Elevated adrenal androgens such as DHEAS – Normal levels of testosterone – You may ovulate regularly. – Accounts for about 10 percent of PCOS diagnoses – Risk Factors: possibly genetic |
All right, we have reviewed the diagnostic criteria and the four subtypes of PCOS, but how does one figure out the driver of their PCOS and targeted treatment approach? The first step would be labs.
What lab work should I have done for PCOS?
The holy grail of hormone testing would be the DUTCH, Dried Urine Test for Comprehensive Hormones. This comprehensive test gives more insight into why you might be experiencing your symptoms. You can order the test online, but it is recommended that you work with a doctor that knows how to interpret the DUTCH. DUTCH does not test the thyroid, so see below for thyroid tests.
The DUTCH is more expensive and is not an option for everyone; you can ask your doctor for the following blood hormone tests. If you are cycling, these tests should be performed 5-7 days after ovulation because they will help you determine proper progesterone levels.
- Estradiol
- Progesterone
The following list is an androgen panel
- Total testosterone
- Free testosterone
- Androstenedione
- DHT
- DHEA-S
The following list of hormones should be tested between cycle days 2 and 4 to get a clearer picture of fertility
- FSH
- LH
- Can be tested near ovulation as well to see if LH is rising appropriately
- Estradiol
The following list of tests can be tested at anytime
- Vitamin D
- Prolactin
- Sex-hormone binding globulin
- Blood sugar markers (glucose tolerance, fasting insulin, fasting glucose, and hemoglobin A1c)
Thyroid testing is also necessary as it plays a massive role in the reproductive and endocrine-metabolic function
- TSH
- Free T4
- Free T3
- Reverse T3
- TPO and TGAB
How do I know what type of PCOS I have?
After reviewing your labs with your doctor, you can use this flow chart from Lara Briden as a quick reference to see where you may fall on the spectrum (Briden, 2022).
What is the treatment for polycystic ovary syndrome?
The treatment for insulin-resistant PCOS is to reverse insulin resistance with diet, exercise, and supplements like magnesium and inositol.
The treatment for post-pill PCOS is to understand that is maybe a normal withdrawal process from the drug. “Menstrual periods typically resume within three months after you stop taking the pill” (Birth Control Pill FAQ, n.d.). You can consider using natural androgen-blocking supplements such as zinc, DIM, or peony & licorice.
The treatment for inflammatory PCOS is to identify and correct the underlying source of inflammation. That could mean avoiding diagnosed food sensitivities, fixing an underlying gut problem, or addressing chronic mast cell activation or histamine intolerance. Per Dr. Lara Briden, “The supplements zinc and N-acetyl cysteine work particularly well for inflammatory PCOS” (Briden, 2022).
Adrenal PCOS is an “epigenetic upregulation of adrenal androgens” (Briden, 2022). Natural Treatments include magnesium, zinc, licorice, adaptogen herbs, and pantothenic acid (vitamin B5), which modulates adrenocorticotropic hormone (ACTH).
What if I have more than one type of polycystic ovary syndrome?
What if you have more than one type? The types are listed in order of priority. So, if you have insulin resistance, then you have insulin-resistant PCOS—even if you also have inflammation and a post-pill worsening of your symptoms. Remember, 70% of women diagnosed with PCOS will have insulin resistance and only 10% will have adrenal PCOS.
In Conclusion
As many as 5 million women have been diagnosed with PCOS in the United States. As more women become diagnosed, more research is being done to understand this condition. Never hesitate to advocate for yourself. Your health is worth it.
References
Birth control pill FAQ: Benefits, risks and choices. (n.d.). Mayo Clinic. Retrieved November 8, 2022, from https://www.mayoclinic.org/healthy-lifestyle/birth-control/in-depth/birth-control-pill/art-20045136
Briden, L. (2022, January 29). 4 types of pcos(A flowchart). Lara Briden – The Period Revolutionary. https://www.larabriden.com/4-types-of-pcos-a-flowchart/
Chang, S., & Dunaif, A. (2021). Diagnosis of polycystic ovary syndrome: Which criteria to use and when? Endocrinology and Metabolism Clinics of North America, 50(1), 11–23. https://doi.org/10.1016/j.ecl.2020.10.002
Khadilkar, S. S. (2016). Polycystic ovarian syndrome: Is it time to rename pcos to ha-pods? Journal of Obstetrics and Gynaecology of India, 66(2), 81–87. https://doi.org/10.1007/s13224-016-0851-9










This is incredible information… thanks for sharing your wealth of education!